 A Nursing Leadership Competency Model
A Nursing Leadership Competency Model
By Rose O. Sherman, RN, EdD, FAAN
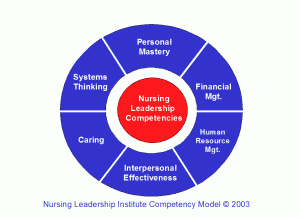
Health care environments today challenge the skills of even the best nursing leaders. Whether it is issues of retaining staff, concern about patient safety, meeting the budget or complying with regulatory rules, more demands are being made of professionals in nursing leadership positions. In 2002, the author conducted research that involved interviews with 120 nursing managers in South Florida to determine their perspective on the leadership skills needed by nursing leaders today. The results of this research were reported in the Journal of Nursing Administration in 2007. Nurse leaders identified personal mastery, interpersonal effectiveness, financial management, human resource management, caring and systems thinking as critical leadership competencies for today’s nursing managers. Here are some of the insights that they shared with us.
Personal Mastery
Leadership skills begin with understanding one’s self. Personal Mastery is a critical component for leadership success. Outstanding leaders demonstrate self-confidence and are able to trust and empower others. They know how their communication and actions impact others and are sensitive to watching the cues in an environment when things are not going well. Nurse managers told us that to be a great leader, your staff needs to have confidence that you are trustworthy and treat everyone fairly. Leaders make mistakes but having personal mastery is being able to look at your mistakes, acknowledge them and learn from them. There is nothing that staff appreciates more than a leader who is able to say “I was wrong”.
Interpersonal Effectiveness
Interpersonal Effectiveness was felt by the managers in our study to be a second key for success. This skill includes not only the ability to communicate, listen and facilitate conflict but also “having a visible presence”. Nursing staff today wants face-to-face contact with their leaders. E-mail is simply not enough. Staff wants to know that they can talk with their managers and feel that they are really being heard and known as individuals. This is a challenge as the average number of staff supervised by an experienced manager in our study was 65 FTE.
Financial Management
Nursing leaders will not survive in their roles if they are not savvy about Financial Management, our third key for success. Most nursing leaders in our study cited this as their weakest area. There is constant pressure to justify the nursing staffing budget, which is a critical part of any hospital’s operating budget. There is now good research to support that higher RN staffing ratios results in better patient outcomes. Proposals that clearly outline the financial benefits of RN staffing models will need to be constructed to make the arguments clear to Chief Financial Officers. The costs of turnover and unfilled beds because of staffing issues need to be quantified and nursing leaders need to have confidence in presenting financial information.
Human Resource Management
The healthcare job market today is a very competitive one. Nursing leaders feel that their ability to do a good job of managing the human resources that they are given has never been more critical. Retention begins with a sound selection and orientation process. The needs and desires of nursing staff in different age groups are often very different. Identifying what motivates staff and keeps them is an important part of their job. Nurse managers in our study told us that it was important for leaders to keep open minds about scheduling, how to best develop staff and what might work as a reward system.
Caring for Staff, Patients and Self
Of all the skills discussed, the managers we interviewed were most passionate about the need to demonstrate that as a leader you care. The ability to maintain a connectedness to staff was a major theme. Whether it means bringing in food or celebrating successes, a great leader cares for his/her staff. Even with 65 FTE, our managers felt they needed to learn about each of their staff and their families. Most told us that they try their best to accommodate the needs of staff for time off or shift schedules. Despite the demands of the nursing leadership role, it is important not to become disconnected from the patients that you care for. Our nurse managers told us that it was important for their staff to see them making rounds on patients. The care of others whether it is staff or patients begins with self-care. This seemed to be a problem area for all but the very seasoned nurse managers that we interviewed. Most of the nursing leaders we interviewed work very long hours and feel very responsible in this era of staffing turbulence to be a resource for their staff at all times.
Systems Thinking
A final skill needed by nursing leaders today is the ability to be a systems thinker. No nursing unit, profession, hospital, healthcare agency or healthcare network is an island today. The healthcare system is interconnected and the challenges confronting the system impact all of us. The nurse managers in our study told us that the most effective nursing leaders are “big picture thinkers”. They make it a point to try to develop a good understanding of how the area that they lead fits into the whole of the organization and respect the perspective of other disciplines. They are proactive in looking at new initiatives such as changes in Medicare reimbursement and HIPAA and assess the impact on the areas that they lead. They look at health policy initiatives and educate their staff, patients and colleagues about the implications of what is being proposed.
Additional Attributes
Two additional attributes that successful nursing leaders demonstrate became clear to us after 120 interviews. The ability to remain optimistic during times of turbulence and the ability to be resilient during times of great change are key ingredients to leadership success.
Read to Lead
Sherman, R.O, Bishop, M., Eggenberger, T., & Karden, R. (2007). Development of a leadership competency model from insights shared by nurse managers. Journal of Nursing Administration, 37(2), 85-94.
Sherman, R.O. 2003. nursing_leadership_model2
© emergingrnleader.com 2011
Are there competencies missing from this model that you believe emerging nurse leaders should work to develop?


 LinkedIn
LinkedIn Instagram
Instagram