 By Rose O. Sherman, EdD, RN, FAAN, NEA-BC
By Rose O. Sherman, EdD, RN, FAAN, NEA-BC
Over the past two years, many health-care agencies in this country have made significant investments in both time and money in the implementation of Electronic Medical/Health records. This implementation phase is just the beginning. As we move into the future, how we use these records will become increasingly more important. Unless the data in these records is used in “meaningful” ways, health-care agencies could be penalized under Medicare reimbursement policies. This will require strategic planning and involvement by nurse leaders. It also requires an understanding of what “meaningful use” of the EMR/EHR in the next stages of implementation is all about.
What is Meaningful Use?
Although electronic medical records have been available for more than a decade, widespread adoption of the EMR/EHR has been very slow. As part of the American Recovery and Reinvestment Act of 2009 (sometimes referred to as the stimulus bill), hospitals and physicians became eligible to receive financial incentives to help finance the cost. Meaningful use is an umbrella term that is used to describe the rules and regulations that are part of the funding act. By 2015, if health-care agencies have failed to implement the electronic record, they will see their reimbursement impacted. So with two years to go, a good question to ask is how are things going? The Office of the National Coordinator (ONC) for Health Information Technology’s has reported that hospital adoption of EHR technology has more than tripled since 2009, increasing from 12.2 percent to 44.4 percent.
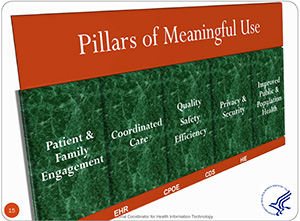
The intent of the policy decisions is not only to promote the widespread use of the EMR/EHR but to also insure that it is being used in a meaning way. There are five goals to meaningful use. The first goal is to improve quality, safety, efficiency and reduce health disparities. The second goal is to engage patients and their families (through electronic communication). The third goal is to improve care coordination. The fourth goal is to ensure adequate privacy and security protection for personal health information. The fifth goal is to improve population and public health on a national level using select measures.
What are the expectations of organizations?
There are three stages in meaningful use and goals for each stage. These include the following:
Stage 1 2011-2012 (many organizations have not yet achieved this stage of electronic data capture and sharing) In this first stage, organizations are expected to capture health information in a standardize format using an EMR. This information should be used to both track key clinical conditions and be available for more effective care coordination. Organizations are also expected to initiate the reporting of clinical quality measures and public health information if they already don’t do thiss. The information captured in the EMR should also be used to engage patients and their families.
Stage 2 2014 (the focus is on more advanced clinical processes)
In stage 2, organizations will be expected to begin participation in health information exchanges (HIE) across organizations and systems. There is also an increased expectation of e-prescribing and incorporating lab results so they are being used in a meaningful way to reduce duplication and avoid errors. If patients move across settings such as from a hospital to a nursing home, the transmission of data should move to being electronic versus paper records. In this stage, patients are expected to be given access to their electronic records and the capacity to review data that is being entered.
Stage 3 2016 (improved outcomes)
During stage 3, the focus moves to using the EMR/EHR to improving patient outcomes. This involves using the electronic record to benchmark best practices, track outcomes and build in clinical support systems for clinicians. Data from the EMR is also expected to be available to provide decision support for national high-priority conditions such as the early identification of a pandemic. Patients will also be expected to be given access to self-management tools and health records that are patient centered. There is great potential to data mine electronic health records with a focus on improving population health.
What are the penalties for not complying?
Although progress at this point is somewhat slow and the time-frames for the stages might be adjusted, ultimately health care agencies and providers will need to comply with the new expectations. Failure to do so may result in stiff penalties with Medicare reimbursement. For providers and health agencies that have not implemented the EHR, there will be a 1% adjustment to Medicare reimbursements that kick in January 1, 2015. The adjustment goes up by 1% each year until 2017 when it becomes 3%. There are also incentives for organizations that have excellent compliance with the meaningful use guidelines.
What does it mean as a nurse leader?
Compliance with the meaningful use goals as they continue to evolve will prove challenging for many organizations – especially smaller agencies with less dedicated IT staff. Nurse leaders will play a key role in helping their organizations in strategic planning. Their input will be especially important in decisions as to to how to best engage patients and transmit data across settings. This is a challenging decade for health care but the implementation of the EHR/EMR is an important step to a better future.
Read to Lead
More Information on Meaningful Use is available at the following 2 websites:
Health IT Government Website http://www.healthit.gov/
Centers for Medicare and Medicare EHR Incentive Program http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/ehrincentiveprograms/
© emergingrnleader.com 2013


 LinkedIn
LinkedIn Instagram
Instagram