By Rose O. Sherman, EdD, RN, NEA, BC
Times of crisis provide an opportunity to test the biases in our thinking. A status quo bias is a preference to keep current practices as they are versus a willingness to think outside the box. A large body of evidence shows that status quo bias frequently affects human decision-making even when under enormous pressure. We love what is familiar and are reluctant to change. Oftentimes we are held back by what we believe to be the safe option, simply because it is our default way of thinking.
An interesting situation now confronting hospitals across the country is their lack of critical care beds and trained staff. The data on COVID-19 admissions is indicating that the majority of patients who need admission will need to be in critical care environments.
In addition to seeking ventilators and potential hospital areas that could be converted, nurse leaders are now considering how to best utilize the nursing resources that they have to staff critical beds with a surge beyond their current capacity. Hospitals in many areas have already stopped all elective surgeries. The volumes on many medical-surgical areas will be down as an outcome of fewer admissions. So how can nurses outside of critical care and the emergency department be effectively deployed to help support these two areas? Part of the answer is expanding our thinking about what staff can do in a time of crisis. We have so often pigeon-holed skill sets and not considered how to rapidly up-skill nurses who won’t have the benefit of a 12-week specialty course in ED or ICU.
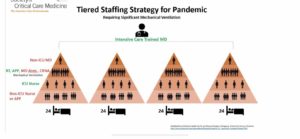
An interesting Tiered staffing model for critical care has emerged from the Society of Critical Care Medicine. They point out that there are 28,808 privileged and 19,996 full-time equivalent intensivists in the United States; however, 48% of acute care hospitals have no intensivists.
This model shows how a medical center could scale up to 96 Critical Care Beds – divided into 24-bed quadrants. Their recommendations include that Intensivists oversee the care of all 96 beds supported by MDs, Nurse Practitioners, PAs and non-intensivist physicians. They recommend that anesthesiologists, nurse anesthetists, and RRTs be deployed on a 1:3 ratio to do ventilator support. The ICU nurse to patient ratio would be 1:6 but critical care nurses would be supported by RNs outside the ICU at a 1:2 patient ratio. Non-critical care staff would need to be quickly trained to provide a supportive role.
While you may want to argue the merits of the model, it is clear that a movement away from status-quo thinking about who can do what and when requires shifting. During this challenging time, nurse leaders cannot be averse to the risk of losing their current reality at the expense of dealing with an evolving pandemic.
Read Rose Sherman’s new book – The Nurse Leader Coach: Become the Boss No One Wants to Leave
© emergingrnleader.com 2020



 LinkedIn
LinkedIn Instagram
Instagram