By Rose O. Sherman, EdD, RN, FAAN
 Intrinsically, we know that the quality of the work environment should impact outcomes. There has been research in this area but none using the level of big data analysis recently done by researchers at Press Gainey as reported by Nell Buhlman in the March 2016 issue of American Nurse Today.
Intrinsically, we know that the quality of the work environment should impact outcomes. There has been research in this area but none using the level of big data analysis recently done by researchers at Press Gainey as reported by Nell Buhlman in the March 2016 issue of American Nurse Today.
They were interested in studying the impact of work environment on key performance measures in the integrated NDNQI data base. This data base includes reporting results from 2000 hospitals on staffing measures, nurse responses to questions about their work environment on NWI practice environment scale, intent to stay and patient outcome measures such as number of falls and ulcers. They also pulled data from the HCAHPS patient satisfaction surveys and publicly reported outcome measures such as 30 readmissions and hospital acquired infections. Researchers looked at the impact staffing, skill mix and work environment on these measures. Across the vast majority of the measures, the performance advantage for hospitals was for those who rated the highest quartile for work environment not those with the highest staffing levels. The study also showed that job enjoyment and intent to stay on a unit (both work environment factors) have greater impact than unit staffing.
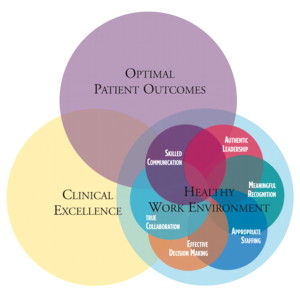
Key Components of a Healthy Work Environment
The American Association of Critical Care Nurses recently updated their widely used work and standards around healthy work environments. They note in their report that studies with their critical care nurse members indicate that moving the needle on work environments has been challenging. In the past five years, their data indicates that nurses believe the quality of their work environments has declined. They identify 6 standards for establishing and sustaining healthy work environments. These include:
1. Skilled Communication – A nurse’s proficiency in communication is as important as clinical skills.
2. True Collaboration – Nurses must be relentless in pursuing and fostering collaboration.that
3. Effective Decision Making – Nurses must be valued and committed partners in making policy, directing and evaluating care and leading organizational operations.
4. Appropriate Staffing – Staffing must ensure the effective match between patient needs and nurse competencies.
5. Meaningful Recognition – Nurses must be recognized and recognize others for the value that each brings to the work of the organization.
6. Authentic Leadership – Nurse Leaders must full embrace the imperative of a healthy work environment, authentically live it and engage others in its achievement.
The Role of Nurse Leaders in Building Healthy Work Environments
The establishment of a healthy work environment requires strong nursing leadership at all levels of the organization but especially at the point of care or unit level where most front line staff work and patient care is delivered. Nurse leaders can help create a deeply satisfying organizational culture at the unit level by engaging staff in the development of shared values in their work. This entails a paradigm shift from a more traditional command and control style of staff supervision toward a more transformational and authentic style of leadership.
Signs of a Healthy Work Environment
So how can you tell if a nursing unit has a healthy work environment? Kramer and Schmalenberg made the important observation from their research that only staff nurses can confirm whether initiatives planned and designed to improve the health of a work environment are truly successful. In their new 2016 guide, the AACN provides a roadmap for nurse leaders of critical elements that should be present for each of the six standards. Wise leaders will download the report and read this important whitepaper.
Read to Lead
American Association of Critical Care Nurses. (2016). AACN HW Standards Updated 2016 (1)
Buhlman, N. (2016). How nurses’ work environment influences key performance indicators. American Nurse Today, 11(3), 54-57.
Kramer, M. & Schmalenberg, C. (2008). Confirmation of a Healthy Work Environment. Critical Care Nurse, 28(3), 56-63.
© emergingrnleader.com 2016


 LinkedIn
LinkedIn Instagram
Instagram